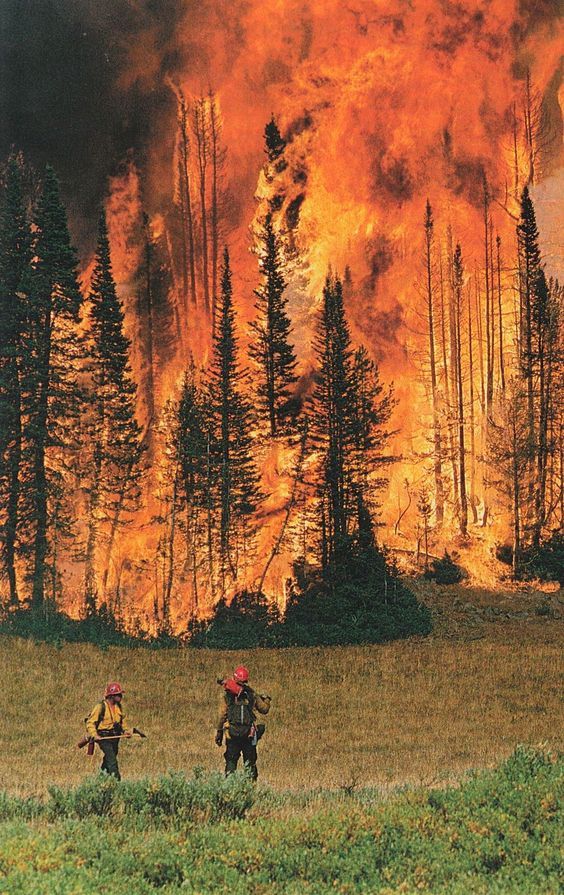
As First Responders of any kind, we know Traumatic Stress well. Our bodies are bombarded 24/7/365, with a continual cascade of stress hormones; even when we are not on call. We are fighting a different kind of war, on home soil!
Due to the heightened awareness of our activated nervous system, that is designed to keep us safe and out of harm’s way, we live in this perpetual state of ‘survival’! Wreaking havoc on our minds, bodies, hearts and relationships.
This miraculous system, our autonomic sympathetic nervous system, also known in the Mammalian Limbic System of the brain, inherited from our ancestors, can go ‘awry’ when placed under this continual, perpetual stress. It’s likened to our adrenaline-cortisol pump being stuck in the ON position. Under normal conditions, when our sympathetic nervous system and limbic brain, get activated under duress, things normalize once the stress has subsided, and the threat is over, returning to homeostasis. However, for those of us that are in these high stress occupations, we don’t get that chance to normalize, keeping us in a continual heightened threat response. Thus, the hypervigilance, insomnia, anger, emotional overload, chronic illness, pain and impatience, especially with loved ones, continues. Although most first responders have tours of duty that help provide time for recovery, it seldom happens, as long as we are back in the saddle again, without addressing the traumatic stress adequately. We are always waiting for the ‘alarm to sound’, even on our days off.
Understanding Traumatic Stress and the effects it has on our bodies and minds, can be so validating. Especially when, one of our survival mechanisms, as first responders, is to compartmentalize our feelings and emotions, which in many cases, can be the difference between life and death during an incident. We don’t have the time, or energy to focus on anything other than the task at hand – the crisis, and the chaos. But what happens when the event is over? What happens when we begin to notice the feelings, thoughts, memories and bodily sensations begin to beg for attention? Like many of us, we may shove them deeper inside, lock them away, throw away the key, determined to never go back there again. Then, we distract ourselves with maladaptive coping mechanisms, also known as ‘emotional junk food’, in order to not FEEL or DEAL with the chaos! And I can tell you this from personal experience, the SHIT will arise, from the very depths of your soul, at some point in your life, if not dealt with appropriately.
What is Traumatic Stress?
Let’s look at Traumatic Stress a little bit deeper. What it is and how we can better prepare ourselves to deal with it? We know that stress is essential to life, however, it’s the type, and duration of the stress, along with our reaction to the stress that is so important. There is the good stress, eustress, and the bad stress, distress. But there’s also the traumatic stress, also known as toxic stress, that is so concerning. It’s like bad stress on steroids! Each time we experience stressors, good or bad, it’s taking another Jenga Block out of the stack. You have this perfectly built, solid foundation, and slowly, one Jenga Block at a time, gets removed, and even stacks back on top. All it takes is that last Jenga Block to get pulled out and the whole stack comes tumbling down; much like Humpty Dumpty.
With first responders, everything we deal with is stressful and traumatic, much of the time. Traumatic stress falls into two categories: environmental and interpersonal. Environmental traumatic stress includes vehicle accidents, medical procedures, war, and natural disasters, to name a few. Whereas, interpersonal traumatic stress is oftentimes, relational, including abuse, neglect, negativity, abandonment, betrayal, shame and rejection.
We also know that traumatic stress affects us: physically, emotionally, mentally, relationally, and spiritually. Traumatic stress can change our views of ourselves and the world, and ourselves in the world, also creating a plethora of associated symptoms and behaviors. For first responders, much like Veteran’s, these events can result in post-traumatic stress or complex post-traumatic stress. I do not refer to them as disorders, diseases, or labels. They are simply, injuries to our sensitive nervous systems.
Post-Traumatic Stress versus Complex Post-Traumatic Stress:
Post-traumatic stress is related to that one-time event, often of shorter duration. The fire, the fatal car accident, the shootout, the bad dispatch call, or medical procedure gone wrong. It leaves a gaping wound in our psyche and body, especially when not addressed timely and properly. The symptoms of PTS include hypervigilance, insomnia, night terrors, terror, flashbacks (visual and emotional) and suicidal ideations. Whereas complex post-traumatic stress occurs when there is continual, ongoing, or cumulative relational stress such as abuse or shame. The abusive spouse, the narcissistic boss, the minimizing friend, or the shaming parent. And we now know that many of us that have experienced PTS pr C-PTS, oftentimes had early development trauma in childhood. (Adverse Childhood Experiences study). C-PTS symptoms are very similar as PTS, but often much more complicated, including self-hate, anger, and self-harming behaviors, and most often, more difficult, and complex to treat.
Sadly, many of us dealing with PTS or C-PTS, oftentimes adopt maladaptive coping mechanisms to deal with the enormous emotional, mental, and physical anguish. Unless you’ve experienced this for yourself, it’s hard to put into words, these invisible wounds. However, the pain and anguish are real! Being able to validate and normalize this experience can be incredibly healing for first responders. And to know that YOU ARE NOT ALONE in your pain.
Some of the maladaptive coping mechanisms, or ‘emotional junk food’, may include:
· Alcohol and Substance Abuse
· Gambling
· Pornography and Infidelity
· Compulsive Shopping
· Workaholism
· Busyness
· Compulsive Exercising
Do any of this sound familiar? What these maladaptive coping mechanisms do to us, and our loved ones is beyond explanation. Traumatic stress breaks up marriages, tears families apart, ruins health, and leaves us feeling hopeless and helpless. However, there is always HOPE! We know that all traumatic stress, when dealt with appropriately, can be healed with time, compassion, trust, safety, and patience. Finding the right healing practitioners and treatment modalities are essential to healing. First and foremost is awareness, the recognition that something is not right, and that you are, indeed, dealing with traumatic stress.
What Can We Do?:
The first step is always PREVENTION and being Proactive. Becoming trauma-informed should be mandatory with all first responders; for yourselves, and the clientele whom you serve. This gives you wisdom, and wisdom gives you power. Having a Traumatic Stress Prevention Plan, that is based on being trauma-informed, should be mandatory in every first responder house, and includes a Suicide Prevention Plan and list of safe and trusted Resources.
The next step is AWARENESS. Awareness, while recognizing the traumatic stress in your lives, and any accompanying symptoms. Being able to recognize when you, or others, might be activated, and knowing what to do, is critical. This is especially important in relation to suicide prevention. Suicidal Ideations are a normal, and common symptom of PTS or C-PTS. Knowing what to do, and not do, can make the difference between life and death. And because our nervous system is already wired to react from a survival standpoint, this is a critical step in knowing your stress response.
Becoming INORMED is a great next step, WISDOM is POWER! Once we have the awareness that something is not right, we can then begin to learn as much as possible, to help better understand and normalize these experiences. However, be very cautious, because there is SO much information out there, especially on the internet, about TRAUMA and GRIEF. It seems as if everyone has a different, and sometimes, contradictory position. It is so important for you to find the practitioners and information that best resonate and make sense to you. What feels right? What doesn’t feel right? Trust that instinct.
Then we look at SUPPORT and Resources. The next most important step is asking for help and be willing to accept it. Every plan should include a list of safe and trusted resources that can be provided to the first responders, and their families. When people are in crisis, they need immediate help and support, they don’t need to be put ‘on hold’. That also applies to post-crisis. Healing takes time, and support is essential to healing. Plus, there is no timeline for healing traumatic stress and grief. This can include the development of a Peer Support system within your house and making sure that these peer supporters are trained properly. Talking to a like-minded peer, who not only understands the job, but has also experienced their own healing journey, is vital.
We can’t forget FOLLOWUP and SELF-CARE.
What happens when all the dust settles, and the traumatic event has ended? Most of the time, people are bombarded with help and support immediately following a crisis, but what happens weeks and months later. This is when follow up is most needed. When the friends and families quit calling or visiting and the shadows begin to surface. That’s why this is the most important time after recovery, especially if you’ve been in any kind of inpatient program. Making sure that you have a system in place to provide follow up and ongoing support.
We, as first responders, are oftentimes so compelled to take care of everyone else, that we easily neglect our own self-care; sometimes referred to as the ‘Savior Complex’. And this oftentimes stems from our own internal wounding. Self-Care should always be a priority, starting with prevention, because everything centers around self-care. It’s easy to distract ourselves through rescuing and taking care of others, but you must put your oxygen mask on first! Some ideas, include:
· Trauma/Grief Therapy, and/or Support Groups
· Trauma-Safe Somatic Movement (yoga, tai chi, qigong, running, hiking, weights)
· Meditation/Mindfulness
· Nature Immersion
· Journaling
· Bodywork: Chiropractic, massage, cranial-sacral, Reiki, acupuncture
· Spiritual Practices: prayer, meditation, Medicine Wheel, chanting, walks in nature and pets
· Spending time with those you love: family and friends
· Community: Spending time with others
· Healing Retreats specific to First Responders
· Service: Giving back, as you are able
In summary, it’s important to remember that YOU ARE NOT ALONE! Over 83% of first responders are dealing with traumatic stress, and the repercussions, when not addressed; can be dangerous. However, it’s part of our first responder culture to ‘suck it up buttercup’ and ‘pull up our fire bootstraps’. However, that’s the machismo of our culture, and can be very destructive if not dealt with appropriately. Remember, YOU ARE YOUR BEST ADVOCATE!! Although you might find responsible and safe people to guide you through this healing journey, you always know what’s best for you. TRUST THAT!
It is my wish and intention that this helps you, or those you love and care for, providing much needed information. I am always available; however, I can be of support.
THANK YOU FOR YOUR SERVICE,
Bequi